About two weeks before her daughter Clementine was due, Kelly Guillou was watching “Mystery Diagnosis” on TV when a story caught her attention. The episode shared the story of a man living with Prader-Willi syndrome (PWS), a rare multi-system genetic disorder.
“I remember thinking what a bizarre syndrome this was, and how hard that must be for the individual and family,” Kelly reflects. While Kelly didn’t know it at the time, the television show’s introduction of PWS was about to become eerily prophetic.
At 41 years old, and already a mother of three, Kelly had been surprised – but delighted – by her pregnancy. “A surprise from the very beginning,” she says with a smile, “who still surprises me to this day.”
And after a relatively uneventful pregnancy, Kelly happily brought her daughter into the world. Although Clementine was small in gestation – a sign Kelly now says would have given her a clue about her daughter’s condition – she seemed healthy at first; her Apgar score was good.
Then doctors began to voice their concerns. Clementine was unusually sleepy; she was hypotonic, meaning she had loose or floppy muscle tone. After being placed in the NICU for two weeks, Clementine underwent rigorous testing.
But Kelly had already heard of the diagnosis – and when the pediatrician called to tell her that Clementine had Prader-Willi syndrome, the same condition Kelly learned about just weeks prior, she was shocked.
At the same time, Kelly was somewhat relieved. She explains: “The doctors had prepared us for if Clementine had a devastating, life-threatening disorder. PWS was the best diagnosis we could have gotten, comparatively.”
In her discussion with Rareatives, Kelly speaks about the complexities of managing Prader-Willi syndrome, why advocacy and research are crucial, and how Clementine is perfect exactly as she is today.
What Comes Next?
As quickly as he delivered the diagnosis, the pediatrician delivered some other discomfiting news: he was completely unfamiliar with Prader-Willi syndrome and could provide the family with no insights beyond that they needed to find someone with more medical knowledge.
Kelly and her family were swept up into online research, a process that Kelly says “is a very common experience for the people in our community.” With a laugh, she says, “Thank goodness for the internet.”
But as much as the internet can bring hope, it can also bring fear. “I’ll be the first to tell you that I struggled mightily when she was first diagnosed,” Kelly tells me. “It came from fear for what the condition might look like for her. Fear for myself, my other children, my husband, my marriage. The fear was tremendous. I felt like I had lost control of my life and it gutted me.”
It was her husband who found the first breakthrough. The world’s leading PWS specialist, Dr. Jennifer Miller, MD, practices at the University of Florida in Gainesville — about a five-hour drive from their home in Atlanta. They immediately called and emailed.

Less than one week later, their efforts paid off. Dr. Miller called the family personally to invite them, and Clementine, to her office. Before they visited, she told them, don’t Google Prader-Willi syndrome – “the information is outdated.”
A weight was lifted, ever so slightly, from Kelly’s shoulders. Says Kelly, “I felt the first glimmer of hope since Clementine was born.”
Dr. Miller provided the family with an exhaustive list of actions and interventions — overwhelming (but welcomed) direction for parents looking to be proactive about care. Most helpful was the information on feeding strategies.
“Many children with PWS experience failure to thrive,” Kelly explains. “Clementine was better in that regard, but it was still difficult to feed her. She was lethargic, slept all around the clock. I had to feed her half to an ounce of breastmilk every 90 minutes because that’s all she could take. She didn’t have the strength to swallow. Most kids have feeding tubes. Clem did not, but that meant that if I wasn’t pumping, I was feeding her – it was all-encompassing.”
The intensive feeding schedule needed to be managed alongside the needs of three other young children — the oldest being five and a half — and Clementine’s feeding, speech, occupational, and physical therapy sessions. Kelly’s husband worked from home, while she was a stay-at-home mom. But despite this fortunate arrangement, there was little respite for either parent.
Even More Unique
The family soon enrolled in Georgia’s Babies Can’t Wait early intervention program. This state program “offers coordinated services for infants and toddlers with special needs, from birth to three years of age, and their families.”
Their home began to fill with people. Every week, three therapists visited for sessions with Clementine. But the situation also required delicate communication from Kelly and their husband to their other children.
“I couldn’t get into too much detail about the diagnosis with the young kids,” Kelly explains. “I wanted them to understand why so much time and energy was being devoted to Clementine, but I didn’t want to frighten them that something was terribly wrong with her. It was like walking a fine line.”
Kelly and her husband simplified their explanation: “She was born a little different. It’s harder for her to roll over or sit up. She’s like you guys though, and still needs your attention and love.”
Early on, Kelly was slightly worried about her children developing resentment, a common concern for parents of children with rare diseases. As Global Genes, a nonprofit organization dedicated to eliminating the burdens and challenges of rare diseases for patients and families globally, explains:
“The siblings may feel guilt that they must not do anything that might add to the burden their parents are already handling. They will likely feel isolated since their life is not like most (or any) of their peers…On the positive side we also see enormous maturity, empathy and compassion in these rare siblings.”
However, Kelly describes her family’s situation as lucky, saying that the siblings adapted well without significant resentment, something Kelly attributes to honest conversation and her children’s innate compassion.
*If you’re searching for support for siblings of those with rare conditions, consider reaching out to the Sibling Support Project or looking at the resources offered by Global Genes’ RARE Disease Siblings Resource Guide.
A Complicating Diagnosis
Prader-Willi syndrome affects an estimated 350,000–400,000 people worldwide. But Clementine’s family soon learned that she is “unique even within an already unique situation.”
When Clementine was eighteen months old, Kelly and her sister – who tagged along to watch Clementine while Kelly immersed herself in the speakers and scientists – attended their first Prader-Willi Syndrome Association | USA (PWSA | USA) national convention in Orlando.
Clementine was fussy – but since she seemed to recover once they returned home, Kelly thought nothing of it. At least, not at first.
Then Clementine began drinking excessive amounts of fluid — as Kelly says, “This is not typical for people with PWS. It’s very difficult to get them to drink water normally.” — and urinating frequently. Soon after, she began losing weight.
Having witnessed similar symptoms in her father, who had semi-recently developed Type 2 diabetes, Kelly recognized the pattern. Despite initial skepticism from her husband and reluctance from their new pediatrician, Kelly insisted on having Clementine tested for diabetes.
A mother’s intuition is always right. But, from the point of Clementine’s Type 1 diabetes diagnosis, a new set of challenges was introduced, including dietary management.
Kelly, smiling, shrugs her shoulders as she says, “Honestly, I wasn’t phased by it. After a PWS diagnosis, it felt mild in comparison. Plus, diabetes is actually a good fit with PWS because the way she needs to eat as a diabetic is very close to how she has to eat with PWS — complex carbs, low sugar, controlled total carbs, whole foods. We had already been feeding her that way.”
The conflict, of course, is that there were five other people in the family, including three children. At events, birthday parties, and holidays, unhealthy eating is part of the experience. To ensure Clementine’s health was protected, Kelly and her family all had to adopt a new diet.
Now, looking back, she sees this as somewhat of a silver lining: “We were forced to become healthier eaters and that’s benefited all of us as we’ve gone through the past 14 years. If we didn’t have to do it, we might not have made those changes.”

The dual diagnosis also made it easier to explain Clementine’s situation to others. Before, when Kelly told people that Clementine had PWS, people would look at her confused. “But tell them she has diabetes,” she says, “and the lightbulb turns on, which helps people understand her restrictions.”
Breaking Outdated Stereotypes about Prader-Willi Syndrome
Kelly emphasizes that public perception around Prader-Willi syndrome remains largely shaped by outdated information. She points to her computer, then follows up with, “If you Google PWS, you would see the same photos that have been out there since 1990. They show people who are very obese or short in stature, which is what we used to see.”
This portrayal is no longer accurate for individuals with PWS treated with growth hormone, which was approved for the condition in June 2000. The physical manifestation has changed. People with PWS are now slimmer and taller, with a different body composition and less dysmorphic features like small hands or feet.
Conversations around hyperphagia are also changing, especially in relation to better understanding hyperphagia and how to treat it. Hyperphagia, a feeling of intense and insatiable hunger, is a characteristic element of Prader-Willi syndrome. Clementine’s doctor told Kelly that she has never seen someone with PWS who does not eventually develop hyperphagia.
When Kelly first read about hyperphagia, the manifestation frightened her. She kept imagining a child that would ask about food around the clock, try and break into the fridge or rash, or run away to get food. “In our case, it’s less severe,” she says, “but it is that extreme for some people.”
That’s why Kelly hopes, in the future, to see an increased research focus on hyperphagia to identify potential interventions that would reduce hyperphagic behavior.

Another misconception around PWS is that hyperphagia is the only disruptive symptom, whereas many parents reference sleep as a particular point of concern. In Clementine’s case, her circadian rhythms were off from birth to age four.
“She would sleep a lot during the day, but would wake up at night. She’d want to come out of her room, play, or see what someone else was doing. Nobody was getting much sleep. Clementine would be exhausted during the day, but she’d have to be participatory at therapy,” Kelly tells me. “Different people have success with different medications. For Clementine, ADHD medication keeps her alert during the day and aids with sleep at night.”
Earlier this year, the family switched insurance companies — and Clementine had to briefly go without her ADHD medication.
“She immediately fell asleep when she got in the car to go to school,” Kelly recounts. “Were she not to be on medication now, she’d have those same struggles. I’d love to see more research done on long-term solutions to sleep issues.”
Addressing the Need for Research and Funding
When Clementine was seven and a half years old, she and her mother traveled to Dr. Miller’s office for an appointment. Dr. Miller made an offhand comment about research she’d like to do if she had the money.
In the rare disease space, research funding requirements often fall squarely on the shoulders of families, patients, and researchers — rare disease does not get the same level of funding as more common conditions.
That didn’t seem fair to Kelly. So she decided, rather than sit back and wait, she would make the change she wanted to see. She started a grassroots fundraising organization to raise money specifically for Dr. Miller’s research.

With a laugh, Kelly says, “I told Clem that she was the face of our fundraising organization. She considers herself to be an influencer now.”
Then, her voice quieting, she adds, “We sometimes think our kids can’t do certain things. But if we put them in a position to build on that, they become more confident and feel better in their own skin. When you ask Clem what she likes about fundraising, she says, ‘I can help other people.’ It’s normal to be overwhelmed in the first few years. If you can make an attempt to reach out to others, to fundraise, to advocate, you’ve empowered yourself, and that empowerment rubs off on your child.”
In the past year, Kelly turned over the fundraising organization to another PWS family with exciting plans for its future. Her own priorities have shifted towards state and federal policy advocacy. She joined the PWS Association of Georgia and took over the state advocacy group to amplify the voices, needs, and rights of the community.
This role recently took her to the Georgia State Capitol for “Wagers and Wavers Day” to advocate for higher wages for service providers who support adults with disabilities through programs like NOW and COMP.
Clementine Today
Now a seventh grader — “fourteen going on forty,” Kelly laughs — at the local public high school, Clementine is thriving in her special ed classroom setting. “School is harder for her, but she tries,” Kelly says.
Of course, there are still elements of PWS that Clementine struggles with. Her PWS manifests most prominently through anxiety, a common but less-discussed aspect of the condition. Kelly describes her daughter’s anxiety as “constant, even when she’s in her room (her happy place) listening to Taylor Swift, which she loves more than anything else.”

The anxiety can lead to behavioral issues such as skin-picking or hair-pulling: behaviors that “wax and wane” but are always there. Clementine also has to know what’s going on, when and how something is going to happen, who is going to be there, and what’ll happen if said event or activity does not happen: “She’ll ask you the same question twenty times if you let her.”
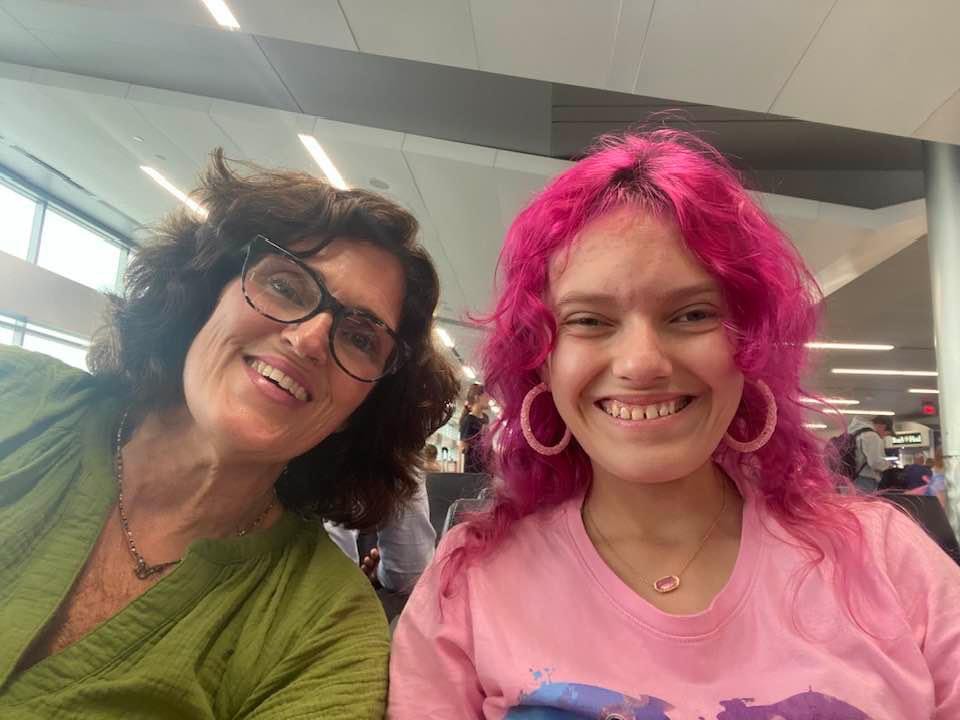
Yet despite these challenges, Clementine takes on life with a full heart and a genuine love for those around her. She adores Taylor Swift, the color pink, traveling, and cats. Kelly describes her as “a lovely person — kind, observant, and honest to a fault.”
“Clementine is perfect as she is right now,” Kelly reflects. “She will be that same person in the future; she has been that person since she was born. She is the interaction of her genetics, environment, and medical conditions — but she is greater than the sum of her parts. PWS is challenging, but it has given gifts to Clem that she wouldn’t otherwise have. She’s tough, resilient, and rolls with the punches. She has confidence. She knows she’s special — not in a bad way, but because she is, and she accepts that.”
Admittedly, it took time for Kelly to reconcile her initial visions for her daughter’s future with the nuances of life with PWS. “But she’s an inspiration to me. She wouldn’t be the same loving, special person without what she’s faced. And now” — a chuckle — “she really is just a typical teenager.”
This normalcy appears in unexpected, and sometimes humorous, ways. Growing up, Clementine watched her older siblings — two of whom no longer live at home, and one who does — sleep in on the weekends. When Clementine turned thirteen, she turned to her parents and declared that “she’s a teenager now and has to sleep.”

This proclamation meant sleeping in on the weekends, to her parents’ delight. Even now, and even if she’s awake, Clementine will not come out of her room until noon. Kelly says, “She is bound or determined. If, for some reason, we have to get her up on the weekend, it better be for a great reason or she’s not having it. She’s funny that way.”
Lessons from the Journey
Candidly, Kelly tells me that for the first few years following Clementine’s diagnosis, all she did was survive. And she knows that there are other parents out there who are doing the same — but they don’t have to. “It’s impossible to do it alone,” she reinforces. “Reach out to other rare parents who know where you’re sitting. They’ve walked in those shoes, and they can commiserate and lift the burden.”
At the same time, Kelly wants to remind people to have hope. Being Clementine’s mother has fundamentally changed her perspective. She considers herself more empathetic, healthier, and a stronger member of the community.
Looking at their journey now, Kelly and her family recognize an inherent truth. Prader-Willi syndrome is part of Clementine’s story, but it is neither the beginning nor the end of it. She is, as Kelly repeats simply and profoundly, “exactly who she’s meant to be.”





Leave a comment